Scroll to:
COVID-19 and Its Relationship with Social and Behavioral Factors in the Population of the Republic of Kazakhstan
https://doi.org/10.35627/2219-5238/2023-31-4-22-29
Abstract
Introduction: In the context of the ongoing COVID-19 pandemic, information about risk factors of the infection is of utmost importance. The objective of our study was to analyze the prevalence of behavioral and social risk factors for COVID-19.
Materials and methods: In October–November 2021, we conducted a cross-sectional study among 1,123 residents of Kazakhstan aged 18 to 69 years. We used a standardized customized STEPS questionnaire that included socio-demographic data, behavioral data, and questions related to COVID-19. The significance of differences in data characterizing qualitative features was determined using 2×2 contingency tables based on the value of Pearson’s χ2 correlation coefficient.
Results: The mean age of the respondents was 44 years; 29 % of them were men and 71 % were women. Among those who had experienced COVID-19, there were more young and middle-aged people (p < 0.05), people with higher education (55.6 %) (p < 0.05), people having 1 to 3 family members (p < 0.05), and those not engaged in moderate physical activity. We found no statistical relationship between smoking and the novel coronavirus disease (p > 0.05). Those who recovered had higher titers of IgM and IgG antibodies. There was a considerable difference in disease incidence between the vaccinated and unvaccinated (p < 0.05) with an odds ratio of 1.661 (95 % CI: 1.275; 2.164).
Conclusions: Our findings can serve as a guide for COVID-19 awareness campaigns aimed at the coronavirus disease prevention conducted by health authorities and mass media. They can also serve as the basis for in-depth studies of the contribution of various factors to the risk of the disease.
For citations:
Urazayeva S.T., Kumar G.B., Tussupkaliyeva K.Sh., Balmagambetova S.K., Urazayeva A.B., Nurmaganbetova G.Zh., Nurmukhamedova Sh.M., Amanshiyeva A.A., Tashimova Zh.K. COVID-19 and Its Relationship with Social and Behavioral Factors in the Population of the Republic of Kazakhstan. Public Health and Life Environment – PH&LE. 2023;31(4):22-29. https://doi.org/10.35627/2219-5238/2023-31-4-22-29
Introduction
On January 30, 2020, the World Health Organization (WHO) declared the outbreak of COVID-19 a public health emergency of international concern [1]. A high pandemic potential of the novel coronavirus strain has led to its rapid spread around the world. According to WHO, as of June 1, 2022, 548.7 million confirmed cases of COVID-19 and 6.3 million deaths have been reported globally [2]. The SARS-CoV-2 virus infects people of different sexes, all age groups, races and nationalities.
Population surveys, which require minimal human resources and can reach a large number of respondents in a short time, are a valuable tool for data collection [3][4]. In the context of the ongoing pandemic of the novel coronavirus disease 2019, information about the risk factors that contribute to the development of lifethreatening conditions is of exceptional importance. More than 90 % of those infected with COVID-19 show mild or no symptoms, while others have severe symptoms leading to fatal outcomes. Age has become a major predictor of disease severity since mortality rates are significantly higher in older patients. Men are more severely affected by the novel coronavirus disease than women, which is probably related to a greater production of type I interferon necessary for an early response to COVID-19 in the latter. Identifying key risk factors and taking appropriate clinical action can make a huge difference in saving the lives of COVID-19 patients.
Today, it is common knowledge that behavioral and environmental factors have the greatest impact on human health. The social environment, bad habits, physical activity, the level of education and income affect the risk and severity of SARS-CoV-2 infection [5][6] The COVID-19 pandemic has posed a number of important practical questions for researchers and the society as a whole, such as what percentage of the population has acquired immunity from previous infection, what is the true prevalence of this infection by region and in individual population groups, what factors have contributed to the disease risk. Such studies, however, have not been conducted among the population of the regions of the Republic of Kazakhstan. In this regard, the purpose of our study was to establish the relationship between behavioral and social factors and the risk of COVID-19 among the population of one of the regions of the Republic of Kazakhstan.
This research was conducted within the National Program for Implementation of Personalized and Preventive Medicine in the Republic of Kazakhstan 2022–2024 realized by Asfendiyarov Kazakh National Medical University, grant number OR12165486.
Materials and methods
In October – November 2021, we conducted a cross-sectional study involving 1,123 adults aged 18 to 69 years, all residing in the Mangystau Region of the Republic of Kazakhstan. Given the expected response rate of 62 % and 40 participants from each cluster needed, we used two-stage cluster sampling, in which 30 primary clusters were selected and then a simple random sample of 65 people was selected from the list of all persons aged 18–69 years living in each cluster. All the respondents gave voluntary informed consent to participate in research. The study was conducted using the standardized STEPS questionnaire [7], which was adapted to local conditions. STEPS includes questions related to socio-demographic and behavioral factors and the history of COVID-19. The adapted questionnaire contained the following sections: general information (9 items), demographic information (9 items), and behavioral indicators (56 items). We have also added five questions related to COVID-19: Have you ever had the novel coronavirus disease? How was it confirmed? Have you been vaccinated against COVID-19? If yes, then what vaccine did you get? How many doses of vaccine did you get? The questionnaire was prepared in Russian and official languages for the respondents to have a choice.
The survey was conducted by trained interviewers from among the medical workers of polyclinics in the Mangystau Region. According to the study protocol, monitoring of data collection was carried out by the project coordinators.
Statistical data processing and analysis were carried out using the Statistica 10 software and included calculation of absolute and relative frequencies. We used the Wald method for computing the 95 % confidence interval and the data were presented as P (95 % CI). The significance of differences in data characterizing qualitative features was determined using 2×2 contingency tables based on the value of Pearson’s χ2 correlation coefficient. The critical value of the significance level (p) when testing statistical hypotheses was taken as 0.05.
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Local Ethics Committee of Asfendiyarov Kazakh National Medical University (Protocol 12 of September 28, 2021).
Results
Description of the participants The study involved 1,123 adults with a mean age of 44 years. Most of the participants were women (71 %) and 56.3 % of them were under 40.
We established that 313 of respondents had already had COVID-19. Most of them (45.3 %) were young (aged 30–49), 25.5 % were middle-aged (aged 50–59), and 19.3 % were elderly (aged 60–69) (p ≤ 0.05). Among the respondents who had recovered from the disease, 174 (55.6 %) had higher and 135 (43.1 %) – secondary education (p < 0.05).
The proportion of married respondents among former COVID-19 cases was the highest (66.5 %, n = 208), while those of single, divorced and widowed were considerably lower: 16.3 %, 10.5 %, and 6.7 %, respectively. Table 1 shows no statistical differences in terms of marital status (p > 0.05).
Table 1. Description of the study participants in terms of their COVID-19 experience
Таблица 1. Характеристика участников по статусу заболевания COVID-19
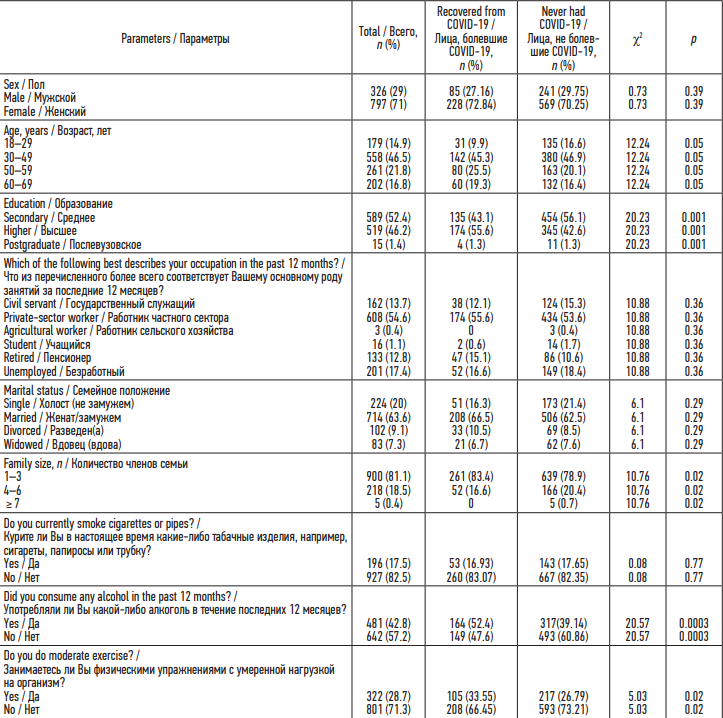
At the same time, we found a statistically significant difference between the disease and the size of the family: among those recovered, the proportion of people having 1 to 3 family members was the highest (p < 0.05).
More former cases of the coronavirus disease were observed among employees of the private sector (55.6 %), unemployed (16.6 %), pensioners (15.1 %), public servants (12.1 %), and students (0.6 %), but the differences between indicators in the socioprofessional groups turned out to be statistically insignificant (p > 0.05).
We established that the majority (208 or 66.45 %) of the respondents with a history of COVID-19 did not go in for sports or exercise and only 105 or 33.55 % exercised at least 10 minutes a day (p < 0.05).
Alcohol consumption was reported by 164 respondents or 52.4 % (p < 0.05) while only 213 respondents or 17.8 % were current smokers. We found no statistical relationship between smoking and the disease (p > 0.05).
We calculated the disease odds ratio in individuals vaccinated against COVID-19 and the unvaccinated and found a significant difference between them (p < 0.05) with an OR of 1.661 (95 % CI: 1.275–2.164).
While COVID-19 was not diagnosed in 80 % of the study participants, they believed that they had had it. In 3.7 %, the disease was diagnosed by a physician based on clinical symptoms and physical examination; in 10.9 % and 3.2 % of cases, it was confirmed by PCR and computed tomography and/or X-ray, respectively, while IgM and IgG antibodies to the SARS-Cov-2 N-protein were found in 2.2 % of the respondents.
Table 2. Odds ratios of the disease among the study participants vaccinated and unvaccinated against COVID-19
Таблица 2. Показатели соотношения шансов заболевания у вакцинированных против COVID-19 и невакцинированных участников исследования
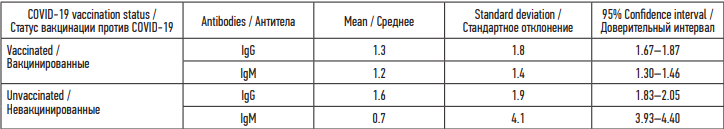
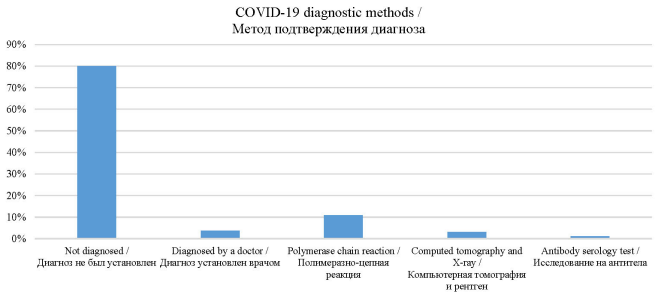
Figure. Distribution of the respondents by the method of diagnosing COVID-19
Рисунок. Распределение респондентов в зависимости от метода установления диагноза
Discussion
The study examined the relationship between socio-demographic factors and the risk of COVID-19. Such factors as sex, age, level of education, size of family, commitment to sports or moderate physical activity, and alcohol abuse can affect the infection rate.
We found that the disease was more frequent among young and middle-aged people aged 30–49 and 50–59 years, respectively.
A study conducted in the United States in 2020 also showed that the incidence of COVID-19 among young people (aged 18–24 years) was higher than in other age groups [8]. According to other investigators, the infection was diagnosed most often in elderly people aged 60+, followed by those aged 45–59 years. In addition, the highest mortality rate was reported in the patients aged 45–59 (55 %), followed by those aged 60 and older (45 %), and the lowest – in the age group of 30 to 44 years (8 %) [9].
The literature review has shown that males are more susceptible to SARS-CoV2 infection, present with a more severe disease, and usually have a worse prognosis [9–11]. A study involving 799 patients at the Tongji Hospital in Wuhan, China found that of 113 deceased patients with coronavirus disease 2019, 27 % were women and 73 % were men [12][13]. The multivariate analysis revealed that male sex was a significant risk factor (OR: 2.206, 95 % CI: 1.012–4.809) for long-term (> 14 days) symptoms of COVID-19 [14]. According to the studies conducted in the USA, among 1,482 patients hospitalized with COVID-19, 74.5 % were aged ≥ 50 years, and 54.4 % were men [15]. The incidence of COVID-19 in men per 100,000 population of Switzerland in the age groups of 60–69 years, 70–79 years and 80+ years as of March 30 was 267, 281 and 477, respectively. Men outnumbered women by 74, 87 and 108 per 100,000 population of Switzerland, respectively. In Germany, the relative differences between men and women were the same [16].
The death toll of the COVID-19 pandemic was especially high in Mexico, where the excess all-cause mortality rate in men was twice as high as that in women. This finding is consistent with previous studies showing that more men die from COVID-19 than women [17][18] and is associated with such factors as smoking and alcohol consumption [19].
The analysis of differences in the level of education among the COVID-19 cases revealed a higher proportion of people with higher education (55.6 % or 174) compared to those with complete secondary education (43.1 % or 135). It can be assumed that the reason for that is the conscious seeking of medical care among those with higher education. The study of cognitive functions in patients with a lower level of education showed, for instance, lower indicators of attention, memory, orientation, and executive functions compared to patients with a higher level of education [20].
We established that COVID-19 was more prevalent in private-sector workers (55.6 %) followed by the unemployed (16.6 %), pensioners (15.1 %), civil servants (12.1 %), and students (0.6 %) but the differences in indicators in socio-professional groups turned out to be statistically insignificant (p > 0.05).
A similar study conducted in St. Petersburg, Russia, showed that the highest level of seropositivity was found in the unemployed (29.5 %), children (29.3 %), healthcare workers (27.1 %), education workers (26.4 %), and businessmen (25.0 %). The lowest level of seroprevalence was observed among military personnel; yet, due to the small sample size, these results should be treated with a certain degree of caution.
At the same time, they require special attention, if confirmed independently, as they may indicate a low involvement of military personnel in the formation of herd immunity to COVID-19, possibly related to the well-known isolation of military personnel from the epidemic process in the city [21].
Commitment to sports or physical exercise has a certain influence on the risk of the coronavirus disease. In our study, of all former COVID-19 cases 208 or 66.45 % did not go in for sports or exercise and 105 or 33.55 % exercised for at least 10 minutes a day. Physical inactivity has an adverse effect on both physical and mental health of a human. It is common knowledge that the COVID-19 pandemic and the related lockdown enforced in many countries of the world have led to a sharp decrease in physical activity of the population, thus inducing exacerbation or chronicity of many hypokinetic diseases and contributing to physical inactivity [22–24]. The results of the Australian population survey showed that “the absence of playing competitive sport and training with friends, teams and within clubs has severely impacted males and younger adults in particular.” Eime et al [25] report that “during COVID-19 lockdown men were significantly more likely than women to report worse or much worse general (p = 0.014), physical (p = 0.015) and mental health (p = 0.038) and lower life satisfaction (p = 0.016). The inactive adults were significantly more likely to report poorer general health (p = 0.001) and physical health (p = 0.001) compared to active adults.”
Among the respondents who experienced COVID-19, 164 or 52.4 % consumed alcohol. Here, it is worth noting an overall increase in alcohol consumption during the pandemic [26]. For example, “the national lockdown implemented in France during the COVID-19 pandemic influenced tobacco and alcohol consumption in different ways according to sociodemographic group and mental health.” Besides, “among alcohol drinkers, 10.7 % reported an increase in their alcohol consumption since lockdown and 24.4 % reported a decrease, while it remained stable for 64.8 %. The increase in alcohol consumption was associated with an age of 18–49 years, living in cities of more than 100,000 inhabitants, a high socio-professional category, and a depressive mood.” [27] In England, the lockdown also led to an increase in alcohol consumption among “high-risk drinkers” (38.3 versus 25.1 %, OR = 1.85, CI = 1.67–2.06) [28].
The study showed that titers of IgM and IgG antibodies to the SARS-CoV-2 N-protein in the recovered were twice as high as those in people who managed to escape from the disease. The results of numerous studies indicate that the IgM response appears earlier than IgG after the SARS-CoV-2 infection, which is consistent with the findings for other pathogens [29–31].
In one of them, antibodies to SARS-CoV-2 (SPIgM and SP-IgG) were detected on the first day of hospitalization in 12.5 % of patients, and SP-IgM peaked after about 22–28 days and became negative in 30 % of patients after 3 months and in 79 % of patients after 7 months after the onset of the disease; IgG peaked around day 22–28, remained high for 4 months, and dropped very sharply at the seventh month [32].
We found a significant difference in the course of the disease between those vaccinated and unvaccinated (p < 0.05) with an odds ratio of 1.661 (95 % CI 1.275; 2.164).
Vaccinated patients with systemic rheumatic diseases and manifestation of COVID-19 have better outcomes compared with unvaccinated individuals with similar disease and treatment characteristics [33].
Peghin et al [34] in their prospective study showed that vaccination against SARS-CoV-2 protects against post-COVID-19 symptoms more than a year after acute infection. The receptor-binding domain (RBD) of SARS-CoV-2 IgG associated with vaccination was not detected in individuals with post-COVID-19 syndrome (> 2,500 U/mL against 0.9–2,500 U/mL; OR: 1.36, 95 % CI, 0.62–3.00, p = 0.441). The presence of non-RBD SARS-CoV-2 IgG induced by natural infection showed a significant association with post-COVID-19 syndrome (OR: 1.35; 95 % CI, 1.11–1.64; p = 0.003).
While COVID-19 was not diagnosed in 80 % of the study participants, they believed that they had had it. In 3.7 %, the disease was diagnosed by a physician based on clinical symptoms and physical examination; in 10.9 % and 3.2 % of cases, it was confirmed by PCR and computed tomography and/or X-ray, respectively, while IgM and IgG antibodies to the SARS-Cov-2 N-protein were found in 2.2 % of the respondents. This finding was consistent with those of other researchers: during the COVID-19 pandemic, 80 % of patients had an asymptomatic or mild course of the disease [35]. A specific feature of COVID-19 is a significant heterogeneity of the humoral response both during the course of the disease and convalescence, and it is far from always possible to associate the seropositivity of the convalescent with the severity of the disease and the duration of the post-infection history. In this regard, the analysis of anamnestic seropositivity to COVID-19 in those who have been ill and who have had or had no contact with COVID-19 patients is of considerable epidemiological significance: among those having never had obvious contact with COVID-19 patients, the proportion of seropositive people was 22.6 %, while among those in contact this rate was almost twice as high (42.1 %) [21].
Conclusions
Such factors such as sex, age, level of education, number of family members, commitment to sports or moderate physical activity, and alcohol abuse can affect the disease frequency. The disease was common among young and middle-aged people, of whom the majority had higher education and did not exercise. Such behavioral risk factors as smoking and alcohol consumption did not significantly affect the risk of infection. For the majority of study participants, the diagnosis of COVID-19 was not confirmed by laboratory tests. Our findings may form the basis for conducting more in-depth studies to assess the contribution of various factors to the risk of the novel coronavirus disease.
Our study had several limitations; first, there were limitations inherent in the design of a cross-sectional study; the results could be affected by subjectivity as they were based on self-reported data; secondly, this was a multicenter study conducted among the population of three large cities and 14 regions of Kazakhstan, but here we describe our findings only for the Mangystau Region.
References
1. Updated WHO recommendations for international traffi in relation to COVID-19 outbreak. World Health Organization; 2020. Accessed June 23, 2020. https://www.who.int/news-room/articles-detail/updated-who-recommendations-for-international-traffic-in-relation-to-covid-19-outbrea
2. WHO Coronavirus (COVID-19) Dashboard. Accessed June 23, 2020. https://covid19.who.int/
3. Geldsetzer P. Use of rapid online surveys to assess people’s perceptions during infectious disease outbreaks: A cross-sectional survey on COVID-19. J Med Internet Res. 2020;22(4):e18790. doi: 10.2196/18790
4. Ali SH, Foreman J, Capasso A, Jones AM, Tozan Y, DiClemente RJ. Social media as a recruitment platform for a nationwide online survey of COVID-19 knowledge, beliefs, and practices in the United States: methodology and feasibility analysis. BMC Med Res Methodol. 2020;20(1):116. doi: 10.1186/s12874-020-01011-0
5. Urazayeva ST, Kumar GB, Tussupkaliyeva KSh, et al. Prevalence of behavioral risk factors for COVID-19 infection. Literature review. Vestnik Kazakhskogo Natsional’nogo Meditsinskogo Universiteta. 2022;(1):466-477. (In Russ.)
6. Bello B, Useh U. COVID-19: are non-communicable diseases risk factors for its severity? Am J Health Promot. 2021;35(5):720-729. doi: 10.1177/0890117121990518
7. World Health Organization. Noncommunicable Disease Surveillance, Monitoring and Reporting. Accessed June 23, 2020. https://www.who.int/teams/noncommunicable-diseases/surveillance/systems-tools/steps
8. Leidman E, Duca LM, Omura JD, Proia K, Stephens JW, Sauber-Schatz EK. COVID-19 trends among persons aged 0–24 years – United States, March 1–December 12, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(3):88-94. doi: 10.15585/mmwr.mm7003e1
9. Ortolan A, Lorenzin M, Felicetti M, Doria A, Ramonda R. Does gender influence clinical expression and disease outcomes in COVID-19? A systematic review and meta-analysis. Int J Infect Dis. 2020;99:496-504. doi: 10.1016/j.ijid.2020.07.076
10. Alghamdi IG, Hussain II, Almalki SS, Alghamdi MS, Alghamdi MM, El-Sheemy MA. The pattern of Middle East respiratory syndrome coronavirus in Saudi Arabia: a descriptive epidemiological analysis of data from the Saudi Ministry of Health. Int J Gen Med. 2014;7:417-423. doi: 10.2147/IJGM.S67061
11. Lakbar I, Luque-Paz D, Mege JL, Einav S, Leone M. COVID-19 gender susceptibility and outcomes: A systematic review. PLoS ONE. 2020;15(11):e0241827. doi: 10.1371/ journal.pone.0241827
12. Li LQ, Huang T, Wang YQ, et al. COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92(6):577-583. doi: 10.1002/jmv.25757
13. Chen T, Wu D, Chen H, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. doi: 10.1136/bmj.m1091
14. Mo P, Xing Y, Xiao Y, et al. Clinical characteristics of refractory coronavirus disease 2019 in Wuhan, China. Clin Infect Dis. 2021;73(11):e4208–e4213. doi: 10.1093/cid/ciaa270
15. Garg S, Kim L, Whitaker M, et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 – COVID-NET, 14 States, March 1–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(15):458–464. doi: 10.15585/mmwr.mm6915e3
16. Gebhard C, Regitz-Zagrosek V, Neuhauser HK, Morgan R, Klein SL. Impact of sex and gender on COVID-19 outcomes in Europe. Biol Sex Differ. 2020;11(1):29. doi: 10.1186/s13293-020-00304-9
17. Bhopal SS, Bhopal R. Sex differential in COVID-19 mortality varies markedly by age. Lancet. 2020;396(10250):532-533. doi: 10.1016/S0140-6736(20)31748-7
18. Griffith DM, Sharma G, Holliday CS, et al. Men and COVID-19: a biopsychosocial approach to understanding sex differences in mortality and recommendations for practice and policy interventions. Prev Chronic Dis. 2020;17:E63. doi: 10.5888/pcd17.200247
19. Cai H. Sex difference and smoking predisposition in patients with COVID-19. Lancet Respir Med. 2020;8(4):e20. doi: 10.1016/S2213-2600(20)30117-X
20. Valdes E, Fuchs B, Morrison C, et al. Demographic and social determinants of cognitive dysfunction following hospitalization for COVID-19. J Neurol Sci. 2022;438:120146. doi: 10.1016/j.jns.2022.120146
21. Popova AYu, Ezhlova EB, Mel'nikova AA, et al. Herd immunity to SARS-CoV-2 among the population in Saint-Petersburg during the COVID-19 epidemic. Problemy Osobo Opasnykh Infektsiy. 2020;(3):124-130. (In Russ.) doi: 10.21055/0370-1069-2020-3-124-130
22. Haileamlak A. Physical inactivity: the major risk factor for non-communicable diseases. Ethiop J Health Sci. 2019;29(1):810. doi: 10.4314/ejhs.v29i1.1
23. Robinson E, Boyland E, Chisholm A, et al. Obesity, eating behavior and physical activity during COVID-19 lockdown: A study of UK adults. Appetite. 2021;156:104853. doi: 10.1016/j.appet.2020.104853
24. Gallo LA, Gallo TF, Young SL, Moritz KM, Akison LK. The impact of isolation measures due to COVID-19 on energy intake and physical activity levels in Australian university students. Nutrients. 2020;12(6):1865. doi: 10.3390/nu12061865
25. Eime R, Harvey J, Charity M, et al. The impact of COVID-19 restrictions on perceived health and wellbeing of adult Australian sport and physical activity participants. BMC Public Health. 2022;22(1):848. doi: 10.1186/s12889-02213195-9
26. Pozdniakova ME, Bruno VV. Alcohol consumption in Russia during the COVID-19 pandemic. Sotsiologicheskaya Nauka i Sotsial’naya Praktika. 2022;10(3(39)):25-44. (In Russ.) doi: 10.19181/snsp.2022.10.3.9195
27. Guignard R, Andler R, Quatremère G, et al. Changes in smoking and alcohol consumption during COVID-19-related lockdown: a cross-sectional study in France. Eur J Public Health. 2021;31(5):1076-1083. doi: 10.1093/eurpub/ckab054
28. Jackson SE, Garnett C, Shahab L, Oldham M, Brown J. Association of the COVID-19 lockdown with smoking, drinking and attempts to quit in England: an analysis of 2019–20 data. Addiction. 2021;116(5):1233-1244. doi: 10.1111/add.15295
29. Yu F, Le MQ, Inoue S, et al. Recombinant truncated nucleocapsid protein as antigen in a novel immunoglobulin M capture enzyme-linked immunosorbent assay for diagnosis of severe acute respiratory syndrome coronavirus infection. Clin Vaccine Immunol. 2007;14(2):146-149. doi: 10.1128/CVI.00360-06
30. Fedorov VS, Ivanova ON, Karpenko IL, Ivanov AV. The immune response to the novel coronavirus infection. Klinicheskaya Praktika. 2021;12(1):33-40. (In Russ.) doi: 10.17816/clinpract64677
31. Saeed AY, Assafi MS, Othman HE, Shukri HM. Prevalence of SARS-CoV-2 IgG/IgM antibodies among patients in Zakho City, Kurdistan, Iraq. J Infect Dev Ctries. 2022;16(7):11261130. doi: 10.3855/jidc.15825
32. Zhou C, Bu G, Sun Y, et al. Evaluation of serum IgM and IgG antibodies in COVID-19 patients by enzyme linked immunosorbent assay. J Med Virol. 2021;93(5):2857-2866. doi: 10.1002/jmv.26741
33. Papagoras C, Fragoulis GE, Zioga N, et al. Better outcomes of COVID-19 in vaccinated compared to unvaccinated patients with systemic rheumatic diseases. Ann Pheum Dis. 2022; 81(7):1013-1016. doi: 10.1136/annrheum-dis-2021-221539
34. Peghin M, De Martino M, Palese A, et al. Post–COVID-19 syndrome and humoral response association after 1 year in vaccinated and unvaccinated patients. Clin Microbiol Infect. 2022;28(8):1140-1148. doi: 10.1016/j.cmi.2022.03.016
35. Syrov AV, Sturov NV, Kolupaev VE. Diagnosing COVID-19 in outpatient practice. Trudnyy Patsient. 2020;18(5):6-9. (In Russ.) doi: 10.24411/2074-1995-2020-10031
About the Authors
S. T. UrazayevaKazakhstan
Saltanat T. Urazayeva, Cand. Sci. (Med.), Assoc. Prof., Head of Department of Epidemiology
68 Maresyev Street, Aktobe, 030019
G. B. Kumar
Kazakhstan
Gaukhar B. Kumar, 2nd year Master of Public Health and Preventive Medicine degree student, Department of Epidemiology
68 Maresyev Street, Aktobe, 030019
K. Sh. Tussupkaliyeva
Kazakhstan
Kymbat Sh. Tussupkaliyeva, Cand. Sci. (Med.), Assoc. Prof., Department of
68 Maresyev Street, Aktobe, 030019
S. K. Balmagambetova
Kazakhstan
Saule K. Balmagambetova, PhD, Assoc. Prof., Department of Oncology
68 Maresyev Street, Aktobe, 030019
A. B. Urazayeva
Kazakhstan
Aisha B. Urazayeva, PhD, Senior Lecturer, Department of Epidemiology
68 Maresyev Street, Aktobe, 030019
G. Zh. Nurmaganbetova
Kazakhstan
Gulaiym Zh. Nurmaganbetova, Master of Medical Sciences, Senior Lecturer, Department of Epidemiology
68 Maresyev Street, Aktobe, 030019
Sh. M. Nurmukhamedova
Kazakhstan
Shara M. Nurmukhamedova, MBA, Lecturer, Department of Epidemiology
68 Maresyev Street, Aktobe, 030019
A. A. Amanshiyeva
Kazakhstan
Aimeken A. Amanshiyeva, MBA, Lecturer, Department of Epidemiology
68 Maresyev Street, Aktobe, 030019
Zh. K. Tashimova
Kazakhstan
Zhuldyz K. Tashimova, MBA, Senior Lecturer, Department of Epidemiology
68 Maresyev Street, Aktobe, 030019
Review
For citations:
Urazayeva S.T., Kumar G.B., Tussupkaliyeva K.Sh., Balmagambetova S.K., Urazayeva A.B., Nurmaganbetova G.Zh., Nurmukhamedova Sh.M., Amanshiyeva A.A., Tashimova Zh.K. COVID-19 and Its Relationship with Social and Behavioral Factors in the Population of the Republic of Kazakhstan. Public Health and Life Environment – PH&LE. 2023;31(4):22-29. https://doi.org/10.35627/2219-5238/2023-31-4-22-29









.png)



























